So, if this is what we are hoping to achieve, how do we overcome the challenges to create integrated care which is more than the sum of its parts?
The panel felt that there was real reason for optimism and an opportunity to be seized. They saw potential for integrated care boards (ICB) and integrated care partnerships (ICP) to make progress if they are properly invested in and well-managed. Despite this, the pace of change needed to achieve effective levels of integration requires a system to be sufficiently agile to adapt rapidly to changing local needs. This calls for a reduction in the layers of complexity present in the current system and the removal of bureaucracy that is hampering progress. The Covid-19 pandemic is a great example of where necessity forced very rapid changes in the healthcare system with rapid digitisation, the introduction of remote appointments, the vaccine rollout, and the design and build of the Nightingale Hospitals just a few examples of fast-tracked processes which would have taken many years to complete without the added impetus. Money flows changed and funding was made available quickly where it was needed; bureaucratic processes were streamlined. A similar fundamental shift in focus would benefit the drive to integrated care.
The challenges around achieving greater integration are complex and, in many cases, the restricting behaviours are engrained. Removing the existing silo mentality and instilling a patient-focused culture, requires purposeful leadership. There needs to be a collective will to integrate, reinforced by continual education, training, and the celebration of success, when it happens. There also needs to be sufficient investment if full commitment is to be expected. Ensuring funding is available and existing money flows are protected, will increase the likelihood of buy-in.
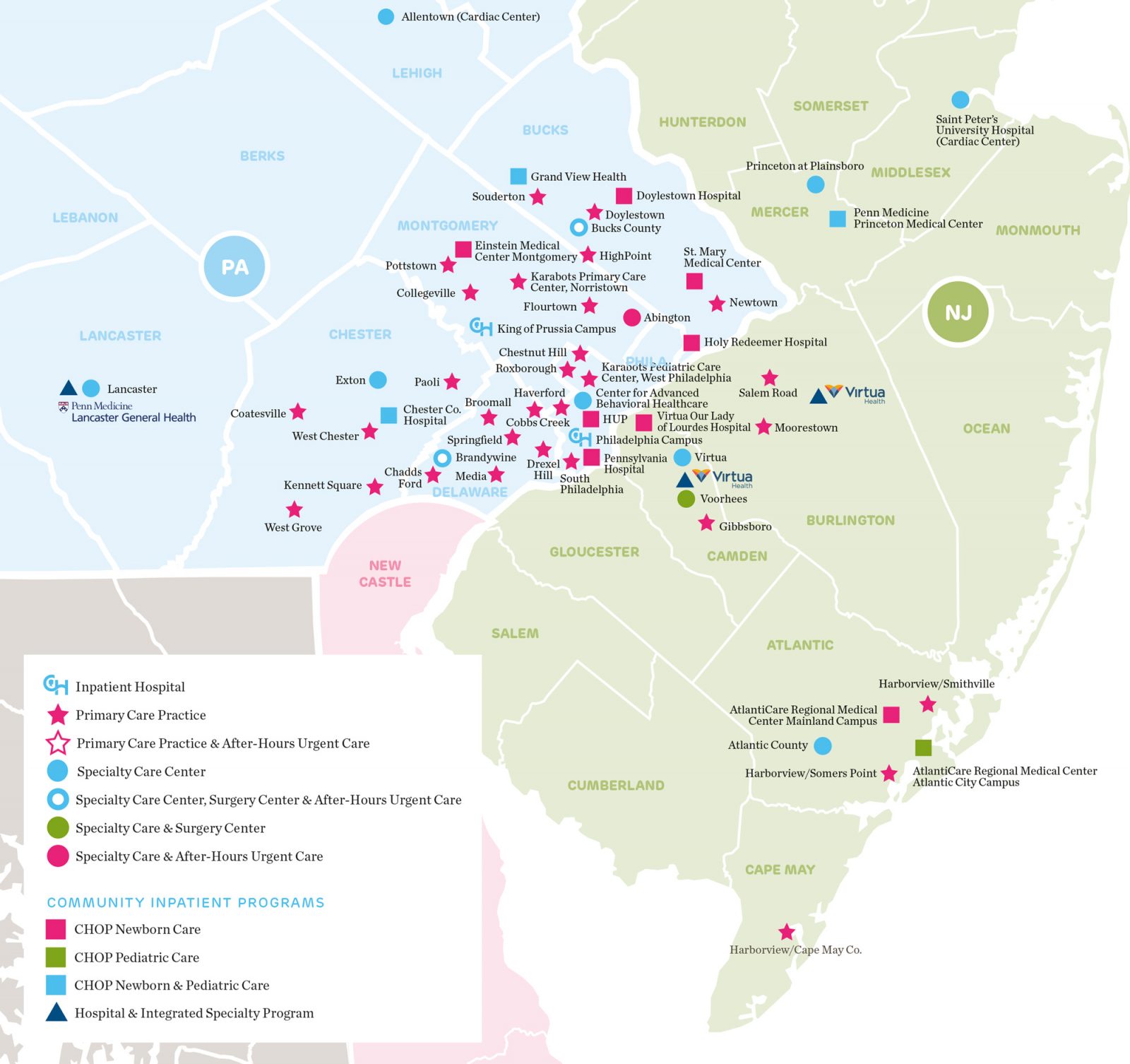
At a more practical level, the panel felt that integrated care is most effective when a place-specific approach is employed. Experience shows that what works well in one part of the country, might not be appropriate in another. Each integrated care partnership will have a different mix of urban vs rural populations, coastal vs inland populations, different demographic and socio-economic landscapes, as well as differences to their existing estates and healthcare services. Public and stakeholder engagement will be key to understand local needs and priorities, and to bring those whose support is most needed, along for the journey. Personal involvement is a great way to overcome resistance to change.
The panel also felt that emphasis would be needed on the deployment of more sophisticated digital solutions to support collaboration, communication, data sharing, and a more efficient delivery of care. It was noted that in many areas the existing IT infrastructure falls well short of where it should for any organisation the size and complexity of the NHS. Tackling existing shortfalls must precede the next stage of technological innovation that will allow integrated care to flourish.
It has been said that in many successful integration initiatives, the role of primary care has been significantly strengthened, with patients working closely with their local GP to take a more proactive approach to their health and wellbeing, alleviating some of the instances of reactive care needed later down the line. The panel felt that a move to nationalise primary care would encourage more medical graduates into primary care and do more to retain the existing talent in the sector.
Finally, the panel discussed the need for greater availability of data in integrated care and for more academic research into the factors that determine success. There is also a need to learn by doing. An iterative process of evidence-based design will highlight the most effective routes to fostering integration. By capturing and distributing examples of best practice the global healthcare community can share an international perspective that may shed new light on this complex challenge.