Combatting loneliness for mental health awareness week
The Mental Health Foundation selected ‘loneliness’ as the theme for this year’s Mental Health Awareness Week. We took this opportunity to reflect on how we create places that cater for planned social interaction and the importance of this in good healthcare design.

Mental healthcare
Of course, privacy and personal space are essential pre-requisites for good mental health recovery. But people are social beings, and the choice of engagement is essential for a sense of wellbeing and autonomy.
In designing mental healthcare settings, a good starting point is to plan a building with a clear sense of what is a private space and what is public realm, and how to arrange the two to provide opportunity and choice. Private bedroom and residential space, for example, may have quiet one-to-one space built into the corridors outside, for low-risk social interaction. We have been pioneers in the use of window seats for this purpose. Smaller and more intimate day rooms can help vulnerable people engage with others whilst still feeling safe.
More public therapy and amenity areas need to cater for larger numbers of people and adopt different characteristics. These places should be designed to encourage people to enter and feel comfortable. Avoiding a sense of ‘enclosure’ is important, being able to spill out to a garden helps people get together without feeling uncomfortable.

Window seating at Clock View Hospital in Liverpool.

Blossom Court in London provides direct access to a courtyard garden from the social day spaces.
Circulation spaces are often overlooked, yet the pattern created here marks out the difference between an environment that isolates and one that fosters social interaction. It is important to offer threshold spaces as a buffer so an individual can make their own choice whether to move into a more complex set of social interactions or not.
Integrated care
A key feature of integrated care is treating people closer to home and the recognition that supporting people in their own dwellings is often much better for quality of life (and more sensible economics) than relocating patients to hospital. Local support and homecare means that an individual stays in a familiar environment, the stress and challenge of relocation is avoided, and delicate, informal social support networks with neighbours and friends are kept intact.
We have pioneered the design of integrated care facilities, including the country’s first, the Jean Bishop Integrated Care Centre in Hull, and we are currently involved in the planning of new classes of primary and community infrastructure in England with Cavell Centres. These bring together a wide range of services and cater for a wider view of wellbeing, with meeting places and facilities to support “social prescribing”, such as gardens and dance space. Here the integration with existing urban and rural communities is central to providing better access to treatment and care closer to home.

The Jean Bishop Integrated Care Centre in Hull.

The centre provides access to gardens to support “social prescribing”.
Acute healthcare
For trauma and many acute health conditions, the acute hospital is the right place to be treated. Although this must be a purposeful clinical environment, social engagement and good communication between patients, staff, and each other, is critical to a good individual experience.
For the patient, although check-in may be automated, a personal welcome is essential for orientation and positive expectations. Clear and unambiguous wayfinding helps reassure, as does the availability of comfortable waiting places.

Refurbished waiting spaces at the Royal Victoria Infirmary in Newcastle upon Tyne.
Consultation space should encourage conversation and good communication, with acoustics and lighting designed to reduce stress. For inpatients, single bedrooms are becoming the norm in new buildings. Here, isolation must be considered, with circulation and dayroom spaces designed to encourage frail patients to move from their room to engage with others. Evidence from the Netherlands shows that this helps speed recovery and combats a sense of loneliness.
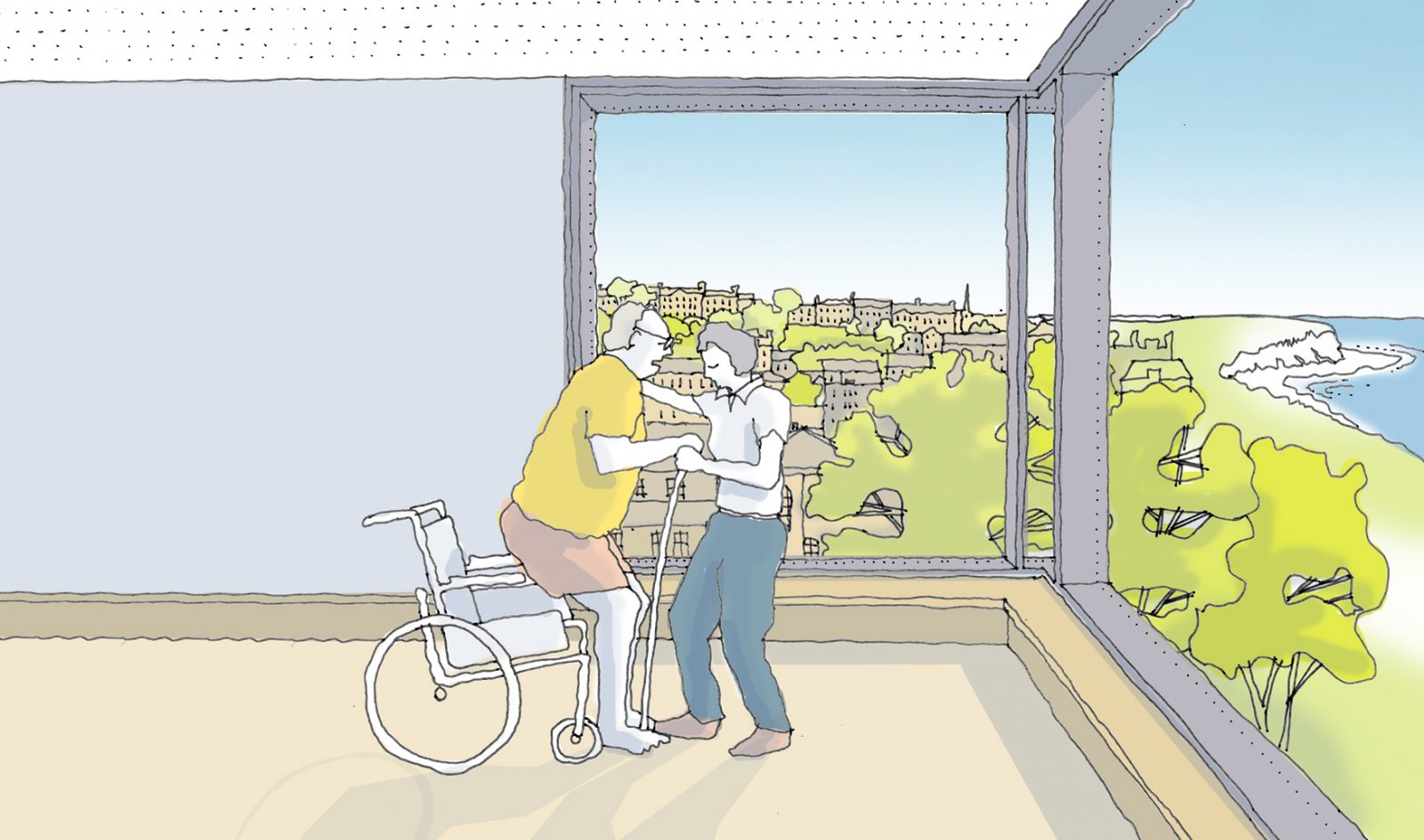
A design for a coastal hospital which provides space for patients to be active, encouraging social interaction.
Staff loneliness should be considered too. Although very busy, really good staff relaxation spaces are very rare in the NHS, and this is a missed opportunity. Consolidating staff areas to provide high quality café, social and professional development space near to treatment areas, not only improves team working and develops a positive organisational culture, but it also provides a setting to encourage social interaction and challenge loneliness.